|
Standardized guidelines for the interpretation of
the fetal heart rate as suggested by the National Institute of Child Health and
Human Development are adopted in the following discussion unless noted otherwise.[2]
The interpretation of the
fetal heart rate tracing should follow a systematic approach with a full
qualitative and quantitative description of the following:
-
Baseline rate
-
Baseline fetal heart rate (FHR) variability
-
Presence of accelerations
-
Periodic or episodic decelerations
-
Changes or trends of FHR patterns
over time
-
Frequency and intensity of uterine
contractions
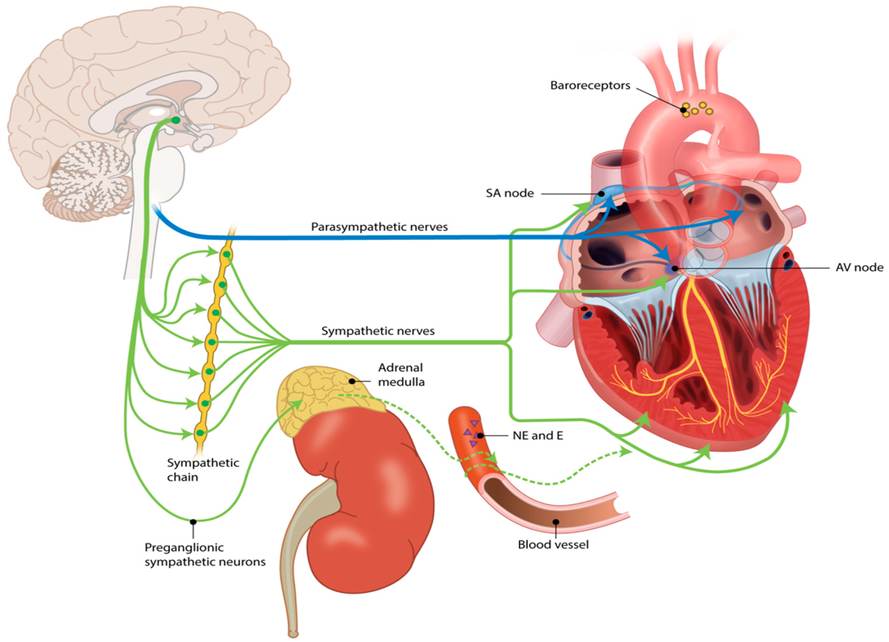
Early in gestation the fetal heart rate is predominantly under
the control of the sympathetic nervous system and arterial chemoreceptors.
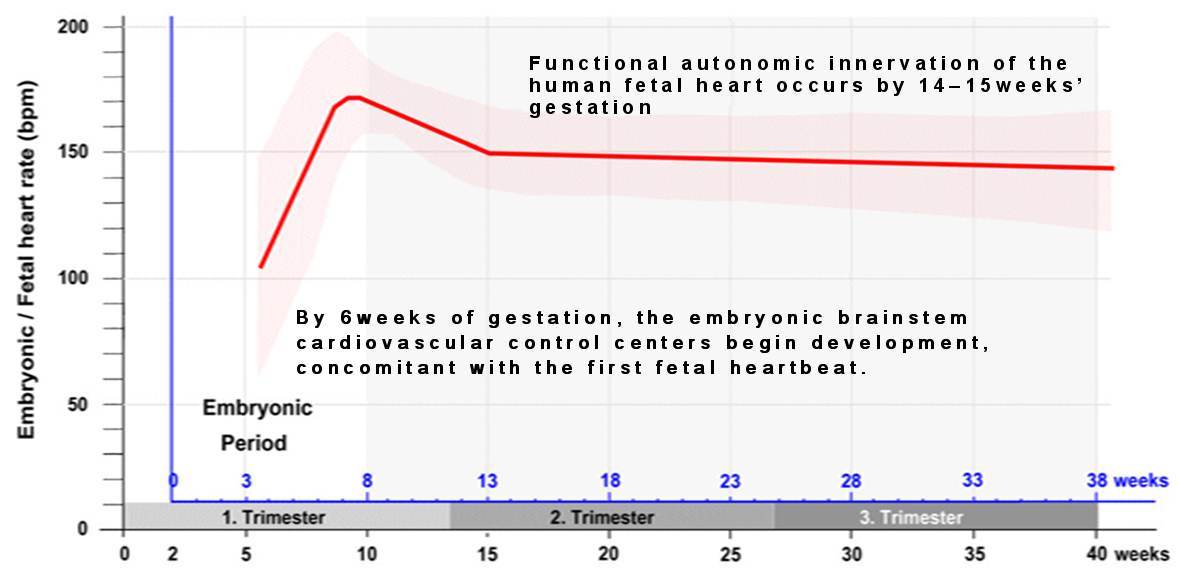
Modified from:Männer, J. When Does the Human Embryonic Heart Start Beating? A
Review of Contemporary and Historical Sources of Knowledge about the Onset of
Blood Circulation in Man. J. Cardiovasc. Dev. Dis. 2022, 9, 187.
https://doi.org/10.3390/jcdd9060187
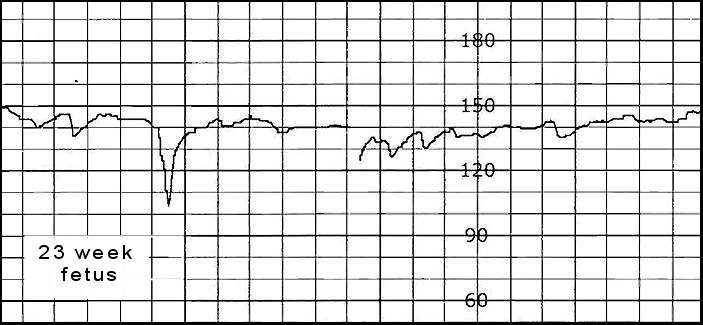
As the fetus develops its heart rate decreases in response to parasympathetic ( vagal stimulation) nervous system maturation and variability becomes more
pronounced [3,4]. Small brief variable decelerations, associated with fetal movement, are common in the fetal heart tracings of premature fetuses [82]
Baseline Fetal Heart Rate (FHR):
"The baseline FHR is the heart rate during a 10 minute segment rounded to the nearest 5
beat per minute
increment excluding periods of marked FHR variability, periodic or episodic
changes, and segments of baseline that differ by more than 25 beats . The baseline FHR in the image above is 130 beats per minute (BPM)
There must be at least 2 minutes of identifiable baseline segments (not necessarily contiguous) in any 10-minute window, or the baseline for that period is indeterminate. If minimum baseline duration is less than 2 minutes then the baseline is indeterminate. In such cases, it may be necessary to refer to the previous 10-minute window for determination of the baseline. The presence of FHR accelerations (either spontaneous or stimulated) reliably predicts the absence of fetal metabolic acidemia" [2]
Bradycardia
:Mean FHR < 110 BPM
-
A rate of 100-119 BPM when accompanied by normal variability and accelerations is not usually a sign of fetal distress.
-
Etiologies:
- Heart block ( < 70 BPM with little or no variability) caused by
structural heart defects (e.g. fetal heterotaxy (left atrial isomerism) , L-transposition of the great arteries, complete AV canal) or anti-Ro/SSA and anti-La/SSB antibodies,
- Hypothermia, maternal heart rate (signal ambiguity) , sinus bradycardia
,cytomegalovirus and parvovirus infection , uterine rupture[5,6, 45, 51, 77]
Tachycardia:
Mean FHR>160 BPM
-
Etiologies:
- Sinus tachycardia (<200 BPM) Maternal fever, fetal anemia,
chorioamnionitis, maternal hyperthyroidism ,terbutaline, hydroxyzine, IV diphenhydramine ,
compensatory sympathetic response to hypoxia caused by stimulation of
catecholamine production by the adrenal gland [50, 52] maternal heart rate (signal ambiguity)
-
Tachyarrhythmias
(usually = or > 200
BPM with abrupt onset little to no variability):(34,35)
- Supraventricular tachycardia (200-240 BPM) accounts for the cause of 70 to 80% tachyarrhythmias and is typically diagnosed at 28 -32 weeks
- Atrial flutter ( atrial rate of 300–600 BPM accompanied by variable degrees of atrioventricular conduction block) the second most common tachyarrhythmia and accounts for 25% of tachyarrhythmias and may be
associated with congenital heart disease. typically diagnosed at 32 weeks , but may be noted at delivery
Baseline change:
The decrease or increase in heart rate lasts for longer than 10 minutes.
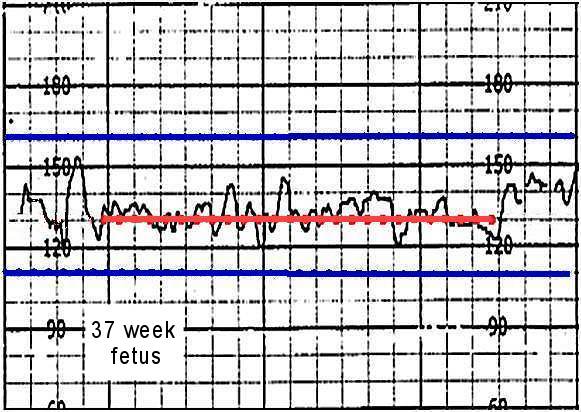
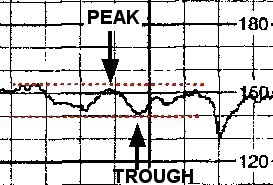
Baseline FHR Variability
Baseline variability is defined as fluctuations in the fetal heart rate of
more than 2 cycles per minute. No distinction is made between short-term
variability (or beat-to-beat variability or R-R wave period differences
in the electrocardiogram) and long-term variability.
Grades of fluctuation are based
on amplitude range (peak to trough):
|
Absent variability = Amplitude
range undetectable
Minimal = < 5 BPM
Moderate = 6 to 25 BPM
Marked = > 25 BPM
The tracing to the right shows an amplitude range of ~ 10 BPM (moderate
variability ).
|
 |
"...in most cases, normal FHR variability provides reassurance about fetal status
and the absence of metabolic acidemia. "[33]
- Etiologies of decreased variability: Fetal metabolic
acidosis (decompensated state) CNS depressants (narcotics) , fetal sleep cycles,
congenital anomalies, prematurity , fetal tachycardia, preexisting
neurologic abnormality, magnesium, betamethasone, cocaine[9-17, 33].
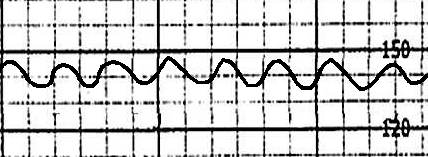
Sinusoidal Heart Rate (SHR)
A SHR pattern is "Visually apparent, smooth, sine wave-like undulating
pattern in FHR baseline with a cycle frequency of 3-5 per minute which persists
for 20 minutes or more.” A SHR has a regular
amplitude and frequency and is excluded in the definition of variability .
This pattern may be generated by fetal sucking movements , central nervous system depressants,Butorphanol, fetal asphyxia/hypoxia, fetal infection, fetal cardiac anomalies, fetal sleep cycles, and
severe fetal anemia.
Modanlou and Freeman proposed that an ominous or "true SHR" , such as that associate with severe fetal anemia, should have no areas of normal FHR variability or reactivity.
Murata et al. were able to obtain a SHR pattern in fetal sheep using chemical or
surgical vagotomy, and arginine vasopressin infusion (a hormone released during
acute blood loss). Power spectral analysis of R-R interval variability suggests the SHR pattern may represent a very
low-frequency component inherent in fetal heart rate variability that appears
as a result of strongly
suppressed autonomic nervous activity. [18-21]
Accelerations
 |
An acceleration is an abrupt increase in FHR
above baseline with onset to peak of the acceleration less than < 30
seconds and less than 2 minutes in duration. The duration of the
acceleration is defined as the time from the initial change in heart
rate from the baseline to the time of return to the FHR to baseline.
Adequate accelerations are
defined as:
-
<32 weeks' : >10 BPM above baseline for
>10 seconds [
-
>32 weeks' : >15 BPM above baseline for > 15 seconds[3].
|
Accelerations are evoked by the sympathetic nervous system Sporadic non episodic accelerations are typically associated with fetal movement. Whereas episodic accelerations are thought to be caused by partial cord occlusion. [23, 32] "The presence of FHR accelerations generally ensures that
the fetus is not acidemic"[24, 33]
Reactivity
:("FHR accelerations that peak (but do not necessarily remain) at least 15 beats per minute above the baseline and last 15 seconds from baseline to baseline."
) [53] is not defined by the NIHCD guidelines.
Prolonged acceleration:
An increase in heart rate that lasts for 2 to 10 minutes.
Periodic or episodic decelerations
Episodic patterns are those
not associated with uterine contractions .
Variable decelerations and accelerations
Periodic patterns are those
associated with uterine contractions.
-
Early and late decelerations
-
Variable decelerations and accelerations
Quantitated by the depth
of the nadir in BPM below the baseline. The duration is quantitated in minutes
and seconds from the beginning to the end of the deceleration. (Accelerations
are quantitated similarly.)
The type of the deceleration
is distinguished on the basis of its waveform.
Gradual decrease and return
to baseline with time from onset of the deceleration to nadir >30
seconds.
-
Further subclassified based on
their relation to the contraction.
Abrupt decrease in FHR of > 15 beats per
minute
with onset of deceleration to nadir < 30 seconds.
|
Early deceleration:
Gradual decrease in FHR
with onset of deceleration to
nadir >30 seconds. The nadir occurs with the peak
of a contraction.
Etiology : Head compression
|
 |
|
Late Deceleration:
Gradual decrease in FHR
with onset of deceleration
to nadir >30 seconds. Onset of the deceleration occurs after the
beginning of the contraction, and the nadir of the contraction occurs after
the peak of the contraction.
Reflect transient or chronic uteroplacental insufficiency
Etiologies : Excessive uterine contractions,
maternal hypotension, maternal hypoxemia (pneumonia),fetal growth restriction, diabetic
ketoacidosis, abruption [56,57, 59]. |
 |
|
Variable:
Abrupt decrease in FHR of >
15 beats per
minute measured from the most recently determined baseline rate
The onset of deceleration
to nadir is less than 30 seconds. The deceleration lasts > 15 seconds and less than 2 minutes.
A shoulder, if present, is not included as part of
the deceleration.
Etiology: Cord compression
Clark SL, et al. define significant variable decelerations as variable
decelerations lasting longer than 60 seconds and reaching a nadir more than 60 BPM below baseline OR reaching a nadir of less than 60 BPM regardless of the baseline [37].
|
 |
Recurrent decelerations ( variable, early,
or late )
Decelerations occur with > 50% of uterine contractions in
any 20 minute segment.
Prolonged deceleration : Defined by NICHD as a
decrease in FHR of > 15 beats per
minute (BPM) measured from the most recently determined baseline rate
The deceleration lasts
>= 2 minutes but less than 10 minutes. The International Federation of Gynecology and Obstetrics (FIGO), defines a prolonged deceleration as a FHR decrease of at least 15 BPM that lasts more than 3 minutes; a prolonged deceleration longer than 5 minutes is considered a pathologic feature [72].
Etiologies:
-
Oxytocin or prostaglandins, maternal
hypotension secondary to supine hypotension or epidural analgesia, umbilical
cord compression secondary to maternal position, rapid descent of the fetal head, [28] artifact (maternal heart rate) " maternal seizure [26]
- "Sentinel Hypoxic or Ischemic Event "such as uterine rupture, severe
abruptio placentae, umbilical cord prolapse, amniotic fluid embolus with
coincident severe and prolonged maternal hypotension and hypoxemia, maternal
cardiovascular collapse, and fetal exsanguination from either vasa previa or
massive fetomaternal hemorrhage [29]
Acidemia has been found to develop after only 2 minutes of a prolonged deceleration [30,54]. Continuation of a prolonged deceleration for 10 minutes or
more is defined by NIHCD guidelines
as a baseline change . Unresolved bradycardia following a
prolonged deceleration before delivery (also known as terminal bradycardia [28] ) has been associated with a higher risk of acidemia.
Despite its association, Cahill AG et. al. found that the presence of unresolved bradycardia prior to delivery was poorly predictive of acidemia with positive predictive value of only 12.9%
in their retrospective study [30]. Williams and Galerneau found decreased variability before FHR bradycardia to be significantly correlated with low umbilical artery pH [55].
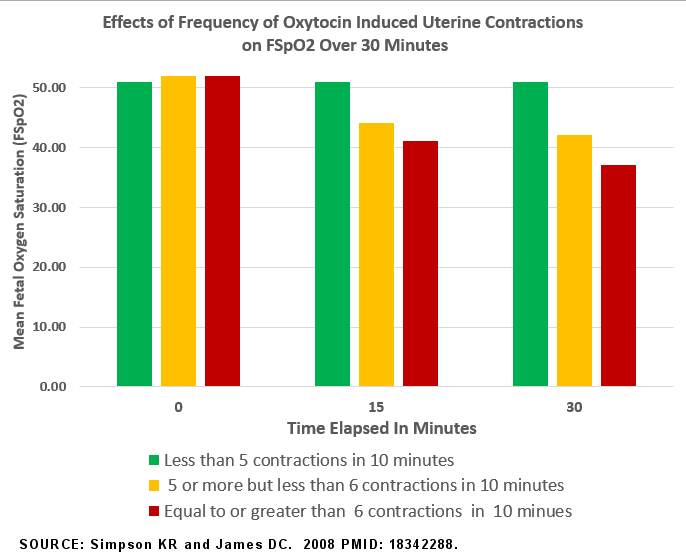
Uterine Contractions Uterine contractions are quantified as the number of contractions present in a 10-minute window, averaged over 30 minutes.
Normal: 5 or less contractions in 10 minutes, averaged over a
30-minute window.
Tachysystole: More than 5 contractions in 10 minutes, averaged
over a 30-minute window. Applies to both spontaneous or stimulated labor. Tachysystole should always be qualified as to the presence or
absence of associated FHR decelerations. Etiologies:Tachysytole may occur
spontaneously, but has been associated with abruption, preeclampsia, epidural , and the use
of oxytocin and / or misoprostol [63, 68]
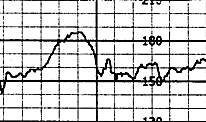
McNamara and Johnson observed that fetal oxygen saturation (FSpO2) drops during contractions in the course of normal labor. FSpO2 reaches its lowest level 92 seconds after the contraction peaks and takes around 90 seconds to return to its initial level. With oxytocin-induced tachysystole, they observed a nearly thirty percent drop in oxygen saturation.
Simpson and James noted a similar decrease in oxygen saturation as well (see graph below). They also observed more periods of absent and minimal variability, less accelerations, more late and recurrent decelerations during oxytocin induced
tachysystole
[64-66]
The terms
hypertonus, hypercontractility, and hyperstimulation
[69,70] are not defined by NIHCD guidelines.
Pathophysiology
Early decelerations appear to be a vagally mediated response to improve cerebral perfusion triggered by an intracranial baroreflex [58, 62].
Late decelerations are brought about by the periodic reduction in perfusion of the intervillous space by uterine contractions.
In the normally oxygenated fetus the decelerations appear to be a vagally mediated reflex to chemoreceptor stimulation (reflex lates) [47].
The lag time to the deceleration after the contraction onset reflects the time for the partial pressure of oxygen (pO2) in the fetal blood to fall to the partial pressure of oxygen (pO2) required to activate the aortic chemoreceptors.
In chronically hypoxic fetuses with decreased variability (decompensated state) late decelerations are probably secondary to hypoxic myocardial depression (non reflex lates). [48, 49].
Variable decelerations are an adaptive response to acute decreases in oxygen
levels during contractions(compression of utero- placental vessels) or cord
compression. When the level of oxygen in the fetal blood is low (hypoxia)
chemoreceptors are triggered causing reflex vagally mediated slowing of the
fetal heart rate that is believed to reduce the myocardial workload, conserving
cardiac glycogen levels, and avoiding the onset of anaerobic metabolism with the
production of lactic acid.
In addition the sympathetic system (including both neural and adrenal components) acts to constrict
blood vessels in nonvital peripheral areas such as the arms and legs to divert
more blood flow to vital organs such as the heart and brain[27]. In the case of
a prolonged deceleration if hypoxia persists the deceleration may be maintained by direct myocardial depression.
[28].
From: Nederend I,
Jongbloed MRM, de Geus EJC, Blom NA, Ten Harkel ADJ. Postnatal Cardiac Autonomic
Nervous Control in Pediatric Congenital Heart Disease. J Cardiovasc Dev Dis.
2016 Apr 15;3(2):16. doi: 10.3390/jcdd3020016. PMID: 29367565; PMCID:
PMC5715679. https://pmc.ncbi.nlm.nih.gov/articles/PMC5715679/
http://creativecommons.org/licenses/by/4.0/).
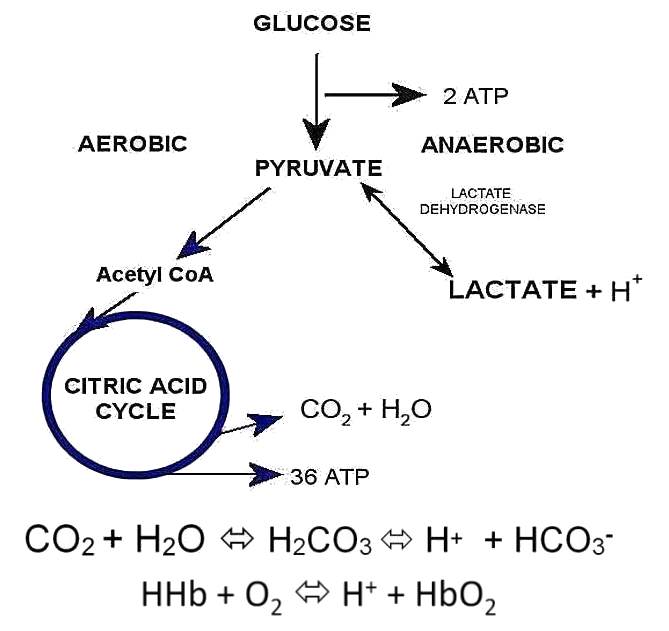
Severe, prolonged, and frequent variables, prolonged uterine contractions, or
prolonged decelerations may not allow enough reperfusion time to adequately eliminate CO2
or restore fetal biochemical status and oxygenation. Persistent hypoxia
leads to the onset of anaerobic metabolism with the generation of lactic
acid . The acid is neutralized primarily by the bicarbonate buffer
system and to a lesser extent by hemoglobin. Without oxygen the lactate
is not metabolized, production of energy (ATP) is minimal, and the buffer
base is consumed by the accumulating acid [30,31,36].
Compromised fetuses may exhibit a
sequence of FHR pattern deterioration characterized by the development of FHR decelerations,
followed by loss of accelerations, then deeper and wider decelerations, followed by a rise of FHR baseline with
frequent episodes of tachycardia or continuous tachycardia, then minimal baseline
variability, and ultimately prolonged decelerations or terminal bradycardia [43]. Matsuda Y
, et. al . observed that "... premature fetuses can quickly develop abnormal heart rate patterns and that these patterns tend to progress in severity much more rapidly than in term fetuses. " [44]
Management
Recommendations have been developed by the American Congress of
Obstetricians and Gynecologists (ACOG) for the interpretation and management of fetal heart rate tracing based on the NICHD
Three-Tier Fetal Heart Rate Interpretation System
Three-Tier Fetal Heart Rate Interpretation System
For Predicting Acid Base Status at the Time of Observation
Category I : Normal. The fetal heart rate tracing shows ALL of the following:
Baseline FHR 110-160 BPM, moderate FHR variability, accelerations may be present or
absent, no late or variable decelerations, may have early decelerations.
Strongly predictive of normal acid-base status at the time of observation.
Routine care.
Category II : Indeterminate.
The fetal heart rate tracing shows ANY of the following:
Tachycardia, bradycardia without absent variability, minimal variability, absent
variability without recurrent decelerations, marked variability, absence
of accelerations after stimulation, recurrent variable decelerations with
minimal or moderate variability, prolonged deceleration > 2 minute but
less than 10 minutes, recurrent late decelerations with moderate variability,
variable decelerations with other characteristics such as slow return to
baseline, and "overshoot".
Not predictive of abnormal fetal acid-base status, but
requires continued surveillance and reevaluation.
Category III: Abnormal.
The fetal heart rate tracing shows EITHER of the following:
Sinusoidal pattern OR absent variability with recurrent late
decelerations,
recurrent variable decelerations, or bradycardia. Predictive of abnormal fetal-acid base status at the time of observation.
Depending on the clinical situation, efforts to expeditiously resolve the underlying cause of the abnormal fetal heart rate pattern should be made.
Algorithms for the Intrapartum Management of Fetal Heart Rate Tracings
“A category II fetal heart rate pattern lasting 60 minutes or more that was identified on initial presentation with persistently minimal or absent variability and lacking accelerations, even in the absence of decelerations, is suggestive of a previously compromised or injured fetus."[75]
Prolonged deceleration
- Perform vaginal exam for impending delivery or cord prolapse if not
contraindicated [46, 72]
- If cord prolapse is present:[71]
- Manual elevation with Trendelenburg (15 degrees),
- Tocolysis if contractions are present.
- If the umbilical
cord is outside of the vagina, warm and moist wrapping should be used to protect the cord
- If possible knee-chest position.
- Fill maternal bladder 500 mL if long-distance transportation or a delay in delivery is expected
- Clear obstacles to rapid delivery
- If an irreversible cause of the deceleration is suspected such as abruption or uterine rupture, or the cause is not
identified and the deceleration persists after 5 or more minutes ,despite corrective measures, then clear
obstacles to rapid delivery
Tachysystole [7, 78]
- Spontaneous labor
- Category I FHR tracing
- Category II or III FHR tracing
- Turn patient to left (preferable) or right lateral position.
- Administer 500 cc LR IV bolus. Consider any fluid restrictions the patient may have.
- If no resolution, consider tocolytic (terbutaline 0.25 mg SC)
- Induction or Augmentation [78]
- Category I FHR tracing
- Turn patient to left (preferable) or right lateral position.
- Administer 500 cc LR IV bolus. Consider any fluid restrictions the patient may have.
- If uterine activity does not return to normal after 10 minutes, decrease the oxytocin rate by at least half; if uterine activity has not returned to normal after 10 more minutes,
discontinue the oxytocin until uterine activity is less than five contractions in 10 minutes
- Category II or III FHR tracing
- Discontinue oxytocin/remove dinoprostone insert/ hold next dose of misoprostol
- Turn patient to left (preferable) or right lateral position.
- Administer 500 cc LR IV bolus. Consider any fluid restrictions the patient may have.
- Administer Oxygen at 10 L/min via nonrebreather mask if the first interventions do not resolve the abnormal FHR pattern. Discontinue oxygen as soon as possible.
- If no resolution, consider tocolytic (terbutaline 0.25 mg SC)
Resumption of oxytocin after discontinuation [78]
If oxytocin has been discontinued for less than 30 minute and the FHR is normal and contraction frequency, intensity, and duration are normal, resume oxytocin at no more than half the rate that caused the tachysystole, and gradually increase the rate as appropriate based on unit protocol and maternal-fetal status.
If oxytocin was discontinued for more than 30 minutes, and the FHR is normal and contraction frequency, intensity, and duration are
normal, resume oxytocin at 1 to 2mU/min."
Assess the oxygen
pathway and consider other causes of FHR changes [60]. Maternal Check maternal 02 sat, Check maternal vitals (fever,
tachycardia) infection , check history of pneumonia, asthma, diabetic ketoacidosis,
hyperthyroidism, maternal blood antibodies, sepsis, and preeclampsia History of drug use (e.g. cocaine, amphetamine) uterine surgery (e.g. cesarean section, myomectomy); Check current medications : terbutaline ,
oxytocin , misoprostol, narcotics, epidural.
Uterus
Check for tachysystole or tetanic contractions, infection, abruption or uterine rupture
Fetus Cord prolapse , fetal anemia, arrhythmia, heart block,
congenital anomaly preexisting neurologic injury , extreme prematurity, growth
restriction .
Corrective measures / Intrauterine resuscitation[7,60,
75, 80].
- Move mother to a lateral position (left or right) to reduce compression of the vena cava and
improve uteroplacental blood flow
- IV fluid bolus of at
least 500 mL lactated Ringer’s solution (if not contraindicated)
- Reduce or discontinue oxytocin
- Modification of pushing efforts (second stage)
- Administer Oxygen at 10 L/min via nonrebreather mask
Pressors (ephedrine 5 to 10 mg IV) if hypotension is present and no response to fluid bolus .
Antibiotic if infection is suspected
Consider amnioinfusion for moderate variable decelerations during first
stage of labor.
Clear obstacles to rapid Delivery [7, 60]
- Evaluate the patient's location and transit time for the operative delivery.
- Prepare the OR or LDR and put the surgical team (surgeon, scrub technician,
and anesthesia personnel) together.
- Obtain informed consent.
- Verify the mother's preparedness (e.g. IV access , Foley).
- Review labs and assess need for availability of blood products
- Verify the fetal variables (presentation, EGA, and EFW).
- Gather neonatal resuscitation staff.
See Also:
UPDATED 3/2/2025 References
1.Westgate JA, et al. The intrapartum deceleration in center stage: a
physiologic approach to the interpretation of fetal heart rate changes in labor.
Am J Obstet Gynecol. 2007 Sep;197(3):236.e1-11. PMID: 17826402
2. Macones GA, Hankins GD, Spong CY, Hauth J, Moore T. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions, interpretation, and research guidelines. Obstet Gynecol. 2008 Sep;112(3):661-6. doi: 10.1097/AOG.0b013e3181841395. PMID: 18757666. PUBMED
3. Renou P, Warwick N, Wood C :Autonomic control of fetal heart rate. Am J Obstet Gynecol 105:949,1969 PUBMED
4. Gagnon R, Campbell K, Hunse C, Patrick J Patterns of human fetal heart rate accelerations from 26 weeks to term. Am J Obstet Gynecol. 1987 Sep;157(3):743-8. PUBMED
5. Spires BP, Towers CV. Fetal Bradycardia in Response to Maternal Hypothermia. Obstet Gynecol. 2020 Jun;135(6):1454-1456. PMID: 32459438.
6. Cabaniss ML Fetal Monitoring Interpretation 2nd ed.Philadelphia, Lippincott Williams & Wilkins, 1993 , p30
7.American College of Obstetricians and Gynecologists. Practice bulletin no. 116: Management of intrapartum fetal heart rate tracings. Obstet Gynecol. 2010 Nov;116(5):1232-40. doi: 10.1097/AOG.0b013e3182004fa9. PMID: 20966730.
8. Hobel CJ Intrapartum clinical assessment of fetal distress. Am J Obstet Gynecol. 1971 Jun 1;110(3):336-42.
PUBMED
9. Paul RH, et. al. Clinical fetal monitoring. VII. The evaluation
and significance of intrapartum baseline FHR variability. Am J Obstet Gynecol.
1975 Sep 15;123(2):206-10.
PUBMED
10.Petrie RH, Yeh SY,
Murata Y, Paul RH, Hon EH, Barron BA, Johnson RJ The effect of drugs on
fetal heart rate variability. Am J Obstet Gynecol. 1978 Feb 1;130(3):294-9.
PUBMED
11. Babaknia A, Niebyl JRThe effect of magnesium sulfate
on fetal heart rate baseline variability. Obstet Gynecol. 1978 Jan;51(1
Suppl):2s-4s.
PUBMED
12. Visser GH, Goodman JD, Levine DH, Dawes GSDiurnal
and other cyclic variations in human fetal heart rate near term. Am J Obstet
Gynecol. 1982 Mar 1;142(5):535-44.
PUBMED
13. Devoe LD Antepartum fetal heart rate testing in
preterm pregnancy. Obstet Gynecol. 1982 Oct;60(4):431-6.
PUBMED
14.Assali NS, Brinkman
CR 3d, Woods JR Jr, Dandavino A, Nuwayhid B Development of neurohumoral
control of fetal, neonatal, and adult cardiovascular functions. Am J Obstet
Gynecol. 1977 Dec 1;129(7):748-59.
PUBMED
15. van der Moer PE,
Gerretsen G, Visser GH Fixed fetal heart rate pattern after intrauterine
accidental decerebration. Obstet Gynecol. 1985 Jan;65(1):125-7.
PUBMED
16 Smith JH, Dawes GS, Redman
CW Low human fetal heart rate variation in normal pregnancy. Br J Obstet
Gynaecol. 1987 Jul;94(7):656-64.
PUBMED
17. Derks JB, Mulder EJ, Visser GH The effects of
maternal betamethasone administration on the fetus. Br J Obstet Gynaecol.
1995 Jan;102(1):40-6.
PUBMED
18. Nijhuis JG, Staisch KJ, Martin CB Jr, Prechtl HF. A sinusoidal-like fetal heart-rate pattern in association with fetal sucking--report of 2 cases. Eur J Obstet Gynecol Reprod Biol. 1984 Jan;16(5):353-8. doi: 10.1016/0028-2243(84)90164-3. PMID: 6705966.
19. Epstein H, Waxman A, Gleicher N, Lauersen NH. Meperidine-induced sinusoidal fetal heart rate pattern and reversal with naloxone. Obstet Gynecol. 1982 Jun;59(6 Suppl):22S-5S. PMID: 7088421.
20. Modanlou HD, Murata Y. Sinusoidal heart rate pattern: Reappraisal of its definition and clinical significance. J Obstet Gynaecol Res. 2004 Jun;30(3):169-80. PMID: 15210038.
21. Suzuki T, et al. Power spectral analysis of R-R interval variability before and during the sinusoidal heart rate pattern in fetal lambs. Am J Obstet Gynecol. 2000 May;182(5):1227-32. PMID: 10819863.
22. lanning Workshop. Am J Obstet Gynecol. 1997
Dec;177(6):1385-90.
23. Sadovsky E, Rabinowitz R, Freeman A, Yarkoni S. The relationship between fetal heart rate accelerations, fetal movements, and uterine contractions. Am J Obstet Gynecol. 1984 May 15;149(2):187-9. doi: 10.1016/0002-9378(84)90196-0. PMID: 6720797
24. Cahill AG, Tuuli MG, Stout MJ, López JD, Macones GA. A prospective cohort study of fetal heart rate monitoring: deceleration area is predictive of fetal acidemia. Am J Obstet Gynecol. 2018 May;218(5):523.e1-523.e12. doi: 10.1016/j.ajog.2018.01.026. Epub 2018 Feb 1. PMID: 29408586; PMCID: PMC5916338.
25 Hon EH, Reid BL, Hehre FW: The electronic evaluation
of the fetal heart rate II. Changes with maternal hypotension. Am J Obstet
Gynecol 79:209, 1960
26.Boehm FH, Growdon
JH Jr The effect of eclamptic convulsions on the fetal heart rate. Am J
Obstet Gynecol. 1974 Nov 15;120(6):851-2.
PUBMED
27. Lear CA, Wassink G, Westgate JA, Nijhuis JG, Ugwumadu A, Galinsky R, Bennet L,
Gunn AJ. The peripheral chemoreflex: indefatigable guardian of fetal
physiological adaptation to labour. J Physiol. 2018 Dec;596(23):5611-5623. doi:
10.1113/JP274937. Epub 2018 Apr 26. PMID: 29604081; PMCID: PMC6265558.
28. Chandraharan E, Ghi T, Fieni S, Jia YJ. Optimizing the management of acute, prolonged decelerations and fetal bradycardia based on the understanding of fetal pathophysiology. Am J Obstet Gynecol. 2023 Jun;228(6):645-656. doi: 10.1016/j.ajog.2022.05.014. PMID: 37270260.
29. Executive summary: Neonatal encephalopathy and neurologic outcome, second edition. Report of the American College of Obstetricians and Gynecologists' Task Force on Neonatal Encephalopathy.
Obstet Gynecol. 2014 Apr;123(4):896-901. doi: 10.1097/01.AOG.0000445580.65983.d2. PMID:24785633
30. Cahill AG, Caughey AB, Roehl KA, Odibo AO, Macones GA. Terminal fetal heart decelerations and neonatal outcomes. Obstet Gynecol. 2013 Nov;122(5):1070-1076. doi: 10.1097/AOG.0b013e3182a8d0b0. PMID: 24104779.
31. Cahill AG, Tuuli MG, Stout MJ, López JD, Macones GA. A prospective cohort study of fetal heart rate monitoring: deceleration area is predictive of fetal acidemia. Am J Obstet Gynecol. 2018 May;218(5):523.e1-523.e12. doi: 10.1016/j.ajog.2018.01.026. Epub 2018 Feb 1. PMID: 29408586; PMCID: PMC5916338
32. Ekengård F, Cardell M, Herbst A. Sporadic accelerations during labor strongly indicate normal pH, whereas periodic accelerations do not: a case-control study. J Matern Fetal Neonatal Med. 2023 Dec;36(1):2157717. d PMID: 36521850.
33. ACOG Practice Bulletin. Intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Number 106, July 2009. Obstet Gynecol 2009;114:192-202
34. Strasburger JF, Prenatal Diagnosis of Fetal Arrhythmias , Clin Perinatol (2005);32(4): pp. 891-912,
35. Larmay HJ, Strasburger JF, Differential Diagnosis and Management of the Fetus and Newborn with an Irregular or Abnormal Heart Rate, Pediatr Clin North Am (2004);51(4): pp. 1033-1050,
36.Tournier A, Beacom M, Westgate JA, Bennet L, Garabedian C, Ugwumadu A, Gunn AJ, Lear CA. Physiological control of fetal heart rate variability during labour: implications and controversies. J Physiol. 2022 Feb;600(3):431-450. 34951476.
37. Clark SL, et al., Intrapartum management of category II fetal heart rate tracings: towards standardization of care. Am J Obstet Gynecol. 2013 Aug;209(2):89-97. doi: 10.1016/j.ajog.2013.04.030. Epub 2013 Apr 27. PMID: 23628263.
38. Raghuraman N, et al Maternal Oxygen Supplementation Compared With Room Air for Intrauterine Resuscitation: A Systematic Review and Meta-analysis. JAMA Pediatr. 2021 Apr 1;175(4):368-376. doi: 10.1001/jamapediatrics.2020.5351. PMID: 33394020; PMCID: PMC7783592.
39. Carbonne B, Benachi A, Lévèque ML, Cabrol D, Papiernik E. Maternal position during labor: effects on fetal oxygen saturation measured by pulse oximetry. Obstet Gynecol. 1996 Nov;88(5):797-800. doi: 10.1016/0029-7844(96)00298-0. PMID: 8885916.
40.Hofmeyr GJ, Lawrie TA. Amnioinfusion for potential or suspected umbilical cord compression in labour. Cochrane Database Syst Rev. 2012 Jan 18;1(1):CD000013. doi: 10.1002/14651858.CD000013.pub2. PMID: 22258939; PMCID: PMC7061253.
41.Leathersich SJ, Vogel JP, Tran TS, Hofmeyr GJ. Acute tocolysis for uterine tachysystole or suspected fetal distress. Cochrane Database Syst Rev. 2018 Jul 4;7(7):CD009770. doi: 10.1002/14651858.CD009770.pub2. PMID: 29971813; PMCID: PMC6513259.
42.Pullen KM, Riley ET, Waller SA, Taylor L, Caughey AB, Druzin ML, El-Sayed YY. Randomized comparison of intravenous terbutaline vs nitroglycerin for acute intrapartum fetal resuscitation. Am J Obstet Gynecol. 2007 Oct;197(4):414.e1-6. doi: 10.1016/j.ajog.2007.06.063. PMID: 17904983.
43. Vintzileos AM, Smulian JC. Decelerations, tachycardia, and decreased variability: have we overlooked the significance of longitudinal fetal heart rate changes for detecting intrapartum fetal hypoxia? Am J Obstet Gynecol. 2016 Sep;215(3):261-4. doi: 10.1016/j.ajog.2016.05.046. PMID: 27568857.
44. Matsuda Y., Maeda T., Kouno S. The critical period of non-reassuring fetal heart rate patterns in preterm gestation. Eur. J. Obstet. Gynecol. Reprod. Biol. 2003;106:36–39. doi: 10.1016/S0301-2115(02)00212-9
45. Karn K, Julian TM, Ogburn PL Jr. Fetal heart block associated with congenital cytomegalovirus infection. A case report. J Reprod Med. 1984 Apr;29(4):278-80. PMID: 6325686.
46. Freeman, Roger K., Thomas J. Garite, Michael P. Nageotte, and Lisa A. Miller . Fetal heart rate monitoring.pp
59,67,68 , 132Lippincott Williams & Wilkins, 2012;
47. Itskovitz J, Goetzman BW, Rudolph AM. The mechanism of late deceleration of the heart rate and its relationship to oxygenation in normoxemic and chronically hypoxemic fetal lambs. Am J Obstet Gynecol. 1982 Jan 1;142(1):66-73. doi: 10.1016/s0002-9378(16)32286-4. PMID: 7055173.
48. Myers RE, Mueller-Heubach E, Adamsons K. Predictability of the state of fetal oxygenation from a quantitative analysis of the components of late deceleration. Am J Obstet Gynecol. 1973 Apr 15;115(8):1083-94. doi: 10.1016/0002-9378(73)90557-7. PMID: 4632417.
49. Harris JL, Krueger TR, Parer JT. Mechanisms of late decelerations of the fetal heart rate during hypoxia. Am J Obstet Gynecol. 1982 Nov 1;144(5):491-6. doi: 10.1016/0002-9378(82)90215-0. PMID: 7137235.
50. Descourvieres L, et al. Types of intrapartum hypoxia in the newborn at term with metabolic acidemia: A retrospective study. Acta Obstet Gynecol Scand. 2022 Nov;101(11):1276-1281. PMID: 36004701
51. Fishman SG,et al.,Parvovirus-mediated fetal cardiomyopathy with atrioventricular nodal disease. Pediatr Cardiol. 2011 Jan;32(1):84-6. PMID: 20936534.
52. Abernathy A, et al.Transient Fetal Tachycardia After Intravenous Diphenhydramine Administration. Obstet Gynecol. 2017 Aug;130(2):374-376 PMID: 28697105.
53. Antepartum Fetal Surveillance: ACOG Practice Bulletin, Number 229. Obstet Gynecol. 2021 Jun 1;137(6):e116-e127. PMID: 34011889.
54. Zilianti M, et al. Studies on fetal bradycardia during birth process. II. Obstet Gynecol. 1973 Dec;42(6):840-3. PMID: 4757590.
55. Williams KP, Galerneau F. Fetal heart rate parameters predictive of neonatal outcome in the presence of a prolonged deceleration. Obstet Gynecol. 2002 Nov;100(5 Pt 1):951-4. PMID: 12423859.
56. Steyn DW, Odendaal HJ. Fetal resuscitation in a patient with varicella pneumonia and preterm labor. Int J Gynaecol Obstet. 1989 Oct;30(2):171-5. PMID: 2572489.
57. Gracia-Perez-Bonfils A, et al. Fetal heart rate changes on the cardiotocograph trace secondary to maternal COVID-19 infection. Eur J Obstet Gynecol Reprod Biol. 2020 Sep;252:286-293. PMID: 32645644; PMCID: PMC7331544.
58. Lear CA, et al. Fetal defenses against intrapartum head compression-implications for intrapartum decelerations and hypoxic-ischemic injury. Am J Obstet Gynecol. 2023 May;228(5S):S1117-S1128. PMID: 34801443.
59. Sibai BM, Viteri OA. Diabetic ketoacidosis in pregnancy. Obstet Gynecol. 2014 Jan;123(1):167-178. PMID: 24463678.
60.. Miller DA.Intrapartum fetal heart rate monitoring: a standardized approach to management. Clin Obstet Gynecol. 2011 Mar;54(1):22-7. doi: 10.1097/GRF.0b013e31820a0564.PMID:21278498
61. Smith H, Peterson N, Lagrew D, Main E. 2016. Toolkit to Support Vaginal Birth and Reduce Primary Cesareans: A Quality
Improvement Toolkit. Stanford, CA: California Maternal Quality Care Collaborative.p149
62. Ball RH, Parer JT. The physiologic mechanisms of variable decelerations. Am J Obstet Gynecol. 1992 Jun;166(6 Pt 1):1683-8; PMID: 1615975.
63.Cabaniss ML Fetal Monitoring Interpretation 2nd ed.Philadelphia, Lippincott Williams & Wilkins, 1993 , p 155
64 McNamara H, Johnson N. The effect of uterine contractions on fetal oxygen saturation. Br J Obstet Gynaecol 1995;102:644-7.
65.Johnson N, Van Oudgaarden E, Montague I, McNamara H. The effect of oxytocin-induced hyperstimulation on fetal oxygen. Br J Obstet Gynaecol 1994;101:805-7.
66. Simpson KR, James DC. Effects of oxytocin-induced uterine hyperstimulation during labor on fetal oxygen status and fetal heart rate patterns.
Am J Obstet Gynecol. 2008 Jul;199(1):34.e1-5. .
67.Simpson KR, James DC. Efficacy of intrauterine resuscitation techniques in improving fetal oxygen status during labor. Obstet Gynecol. 2005 Jun;105(6):1362-8. PMID: 15932830
68. Heuser CC, et al., Tachysystole in term labor: incidence, risk factors, outcomes, and effect on fetal heart tracings. Am J Obstet Gynecol. 2013 Jul;209(1):32.e1-6. Erratum in: Am J Obstet Gynecol. 2014 Feb;210(2):PMID: 23571133.
69. Department for Health and Wellbeing, Government of South Australia. South Australian Perinatal Practice Guideline Tocolysis for Uterine Hypercontractility accessed 1/25/2025
70. The Royal Australian and New Zealand College of Obstetricians and Gynaecologistsntrapartum Fetal Surveillance Clinical Guideline – Fourth Edition 2019 accessed 1/25/2025
https://ranzcog.edu.au/wp-content/uploads/Intrapartum-Fetal-Surveillance.pdf
71.Wong, Lo et al.Umbilical cord prolapse: revisiting its definition and management
American Journal of Obstetrics & Gynecology, Volume 225, Issue 4, 357 - 366 PMID: 34181893.
72. Ayres-de-Campos D, Spong CY, Chandraharan E; FIGO Intrapartum Fetal Monitoring Expert Consensus Panel. FIGO consensus guidelines on intrapartum fetal monitoring: Cardiotocography. Int J Gynaecol Obstet. 2015 Oct;131(1):13-24. PMID: 26433401.
73. Smith H, Peterson N, Lagrew D, Main E. 2016. Toolkit to Support Vaginal Birth and Reduce Primary Cesareans: A Quality Improvement Toolkit. Stanford, CA: California Maternal Quality Care Collaborative.p149
74. ACOG Clinical Practice Update: Update on Criteria for Suspected Diagnosis of Intraamniotic Infection. Obstetrics & Gynecology 144(1):p e17-e19, July 2024. | D
75. Executive summary: Neonatal encephalopathy and neurologic outcome, second edition. Report of the American College of Obstetricians and Gynecologists' Task Force on Neonatal Encephalopathy.
Obstet Gynecol. 2014 Apr;123(4):896-901. PMID:24785633
75. Simpson KR, James DC. Efficacy of intrauterine resuscitation techniques in improving fetal oxygen status during labor. Obstet Gynecol. 2005 Jun;105(6):1362-8. doi: 10.1097/01.AOG.0000164474.03350.7c. PMID: 15932830./font>
76.Ephedrine Package Insert
https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=2c203482-8a04-40fc-93d2-74b30dec7742&audience=professional
77.Ridgeway JJ, et al Fetal heart rate changes associated with uterine rupture. Obstet Gynecol. 2004 Mar;103(3):506-12. PMID: 14990414.
78. Safe Medication Administration: Oxytocin. Content last reviewed July 2023. Agency for Healthcare Research and Quality, Rockville, MD.
https://www.ahrq.gov/patient-safety/settings/labor-delivery/perinatal-care/modules/strategies/medication/tool-safe-oxytocin.html
79. Oxytocin Injection package insert.https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=a9b62187-4141-487c-a9da-f42ad7f9b408&audience=professional
80. Carbonne B, et al., Maternal position during labor: effects on fetal oxygen saturation measured by pulse oximetry. Obstet Gynecol. 1996 Nov;88(5):797-800. PMID: 8885916.
81. OʼBrien-Abel N. Clinical Implications of Fetal Heart Rate Interpretation Based on Underlying Physiology. MCN Am J Matern Child Nurs. 2020 Mar/Apr;45(2):82-91. PMID: 31714283.
82. Sorokin Y, Dierker LJ, Pillay SK, Zador IE, Schreiner ML, Rosen MG. The association between fetal heart rate patterns and fetal movements in pregnancies between 20 and 30 weeks' gestation. Am J Obstet Gynecol. 1982 Jun 1;143(3):243-9. doi: 10.1016/0002-9378(82)90812-2. PMID: 7081342.
|

